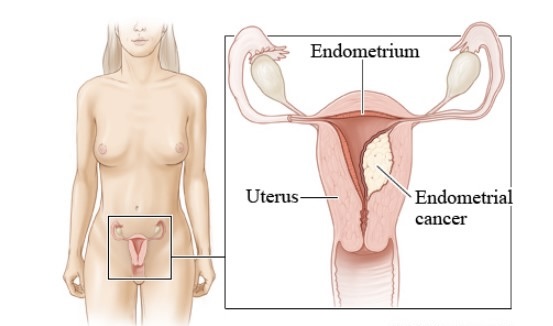
Endometrial Cancer: Symptoms, Causes & Treatment
What are the symptoms of endometrial cancer?
Endometrial cancer, also known as uterine cancer, often presents with symptoms that can be subtle or easily overlooked. The most common symptom is abnormal vaginal bleeding, especially in postmenopausal women. Other symptoms may include:
- Abnormal Vaginal Bleeding: This includes bleeding between periods, heavier or longer menstrual periods than usual, or bleeding after menopause.
- Pelvic Pain: This can occur in the pelvis area, lower abdomen, or lower back.
- Painful Urination: This can be a symptom if the cancer has spread to the bladder.
- Painful Intercourse: This can occur due to the tumor pressing on surrounding organs.
- Unintended Weight Loss: Weight loss without trying can be a symptom of advanced endometrial cancer.
- Fatigue: Feeling tired or lacking energy, which can be a symptom of advanced cancer.
- Other Symptoms: Less common symptoms may include bloating, changes in bowel habits, and a feeling of fullness in the abdomen.
It’s important to note that these symptoms can be caused by conditions other than endometrial cancer. However, if you experience any of these symptoms, especially if they are persistent or unusual for you, it’s important to see your healthcare provider for evaluation. Early detection and treatment can improve outcomes for endometrial cancer.
What are the causes of endometrial cancer?
Endometrial cancer, also known as uterine cancer, develops when cells in the lining of the uterus (endometrium) grow uncontrollably. The exact cause of endometrial cancer is not known, but several factors may increase the risk of developing the disease:
- Hormonal Imbalance: Changes in hormone levels, particularly an excess of estrogen relative to progesterone, can increase the risk of endometrial cancer. This imbalance can occur due to various factors, such as obesity, hormone therapy, or conditions that affect hormone levels.
- Obesity: Obesity is a significant risk factor for endometrial cancer, as excess fat tissue can produce additional estrogen, increasing the risk of abnormal cell growth in the endometrium.
- Age: Endometrial cancer most commonly occurs in postmenopausal women, with the majority of cases diagnosed in women over 50 years old.
- Endometrial Hyperplasia: This condition involves an overgrowth of cells in the endometrium, which can increase the risk of developing endometrial cancer.
- Family History: A family history of endometrial or colorectal cancer may increase the risk of developing endometrial cancer.
- Hereditary Conditions: Certain hereditary conditions, such as Lynch syndrome (hereditary nonpolyposis colorectal cancer or HNPCC), can increase the risk of endometrial cancer.
- Estrogen Therapy: Prolonged use of estrogen-only hormone replacement therapy (HRT) without progesterone can increase the risk of endometrial cancer.
- Tamoxifen Therapy: Tamoxifen, a medication used to treat breast cancer, has been associated with an increased risk of endometrial cancer, particularly in postmenopausal women.
- Diabetes: Women with diabetes may have an increased risk of endometrial cancer, possibly due to insulin resistance and associated hormonal changes.
- Menstrual History: Early onset of menstruation (before age 12) or late menopause (after age 55) can increase the risk of endometrial cancer.
It’s important to note that having one or more risk factors does not mean that a person will develop endometrial cancer. Many women with one or more risk factors never develop the disease, while some women with no known risk factors do develop endometrial cancer. Regular screenings and early detection can help diagnose endometrial cancer at an early stage, when treatment is most effective.
What is the treatment for endometrial cancer?
The treatment for endometrial cancer depends on several factors, including the stage of the cancer, the grade of the tumor, the woman’s age and overall health, and her preferences for treatment. Common treatment options for endometrial cancer may include:
- Surgery: The primary treatment for most stages of endometrial cancer is surgery to remove the uterus (hysterectomy) and often the fallopian tubes and ovaries as well (salpingo-oophorectomy). In some cases, a lymph node dissection may also be performed to determine if the cancer has spread to nearby lymph nodes.
- Radiation Therapy: Radiation therapy uses high-energy beams to kill cancer cells. It may be used before surgery (neoadjuvant therapy) to shrink the tumor, after surgery (adjuvant therapy) to kill any remaining cancer cells, or as the primary treatment for women who are not candidates for surgery.
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells. It may be used in combination with radiation therapy (chemoradiation) for certain stages of endometrial cancer or as adjuvant therapy after surgery to reduce the risk of cancer recurrence.
- Hormone Therapy: Hormone therapy may be used for women with advanced or recurrent endometrial cancer that is hormone receptor-positive. This treatment involves the use of medications that block the effects of estrogen or lower estrogen levels in the body.
- Targeted Therapy: Targeted therapy uses drugs that target specific abnormalities in cancer cells. It may be used in combination with chemotherapy for certain types of endometrial cancer.
- Clinical Trials: Clinical trials may be available for women with endometrial cancer. These trials test new treatments or treatment combinations to determine their effectiveness and safety.
The choice of treatment will be individualized based on the specific characteristics of the cancer and the woman’s overall health and preferences. It’s important for women with endometrial cancer to discuss their treatment options with a multidisciplinary team of healthcare providers, including gynecologic oncologists, radiation oncologists, medical oncologists, and other specialists, to determine the most appropriate treatment plan. Early detection and treatment can improve outcomes for women with endometrial cancer.