Microangiopathic Hemolytic Anemia: Symptoms, Causes, Treatment
What are the symptoms of microangiopathic hemolytic anemia?
Microangiopathic hemolytic anemia (MAHA) is a condition characterized by the destruction of red blood cells (hemolysis) in small blood vessels (microvasculature), often due to mechanical injury. The symptoms of MAHA can vary depending on the underlying cause and the severity of the condition, but may include:
- Fatigue: Due to the decreased number of red blood cells, which carry oxygen throughout the body.
- Pale skin (pallor): Another result of decreased red blood cell count.
- Shortness of breath: Resulting from decreased oxygen-carrying capacity of the blood.
- Jaundice: A yellowing of the skin and eyes due to the breakdown of red blood cells and release of bilirubin.
- Dark urine: Resulting from the breakdown of red blood cells and release of hemoglobin.
- Enlarged spleen (splenomegaly): The spleen may become enlarged as it works to filter and remove damaged red blood cells from circulation.
- Purpura: Small, purplish spots or bruises on the skin caused by bleeding under the skin.
- Increased heart rate (tachycardia): The heart may beat faster to compensate for the decreased oxygen-carrying capacity of the blood.
- Abdominal pain: In cases where the underlying cause of MAHA is related to conditions such as thrombotic thrombocytopenic purpura (TTP) or hemolytic uremic syndrome (HUS), abdominal pain may occur due to the involvement of the gastrointestinal system.
- Neurological symptoms: In severe cases, MAHA can lead to neurological symptoms such as confusion, seizures, or coma. These symptoms may occur if the brain does not receive enough oxygen due to decreased red blood cell count.
It’s important to note that MAHA is a serious condition that requires prompt medical attention by a medical specialist. The underlying cause of MAHA must be identified and treated to prevent further complications and manage the symptoms. Treatment may include addressing the underlying cause, supportive care to manage symptoms, and, in some cases, procedures such as plasma exchange or blood transfusion.
What are the causes of microangiopathic hemolytic anemia?
Microangiopathic hemolytic anemia (MAHA) is caused by conditions that lead to the mechanical destruction of red blood cells (hemolysis) as they pass through small blood vessels (microvasculature). The most common causes of MAHA include:
- Thrombotic thrombocytopenic purpura (TTP): TTP is a rare blood disorder characterized by the formation of blood clots in small blood vessels throughout the body. These clots can damage red blood cells as they pass through the vessels, leading to hemolysis.
- Hemolytic uremic syndrome (HUS): HUS is a condition characterized by the formation of blood clots in the small blood vessels of the kidneys. Similar to TTP, these clots can damage red blood cells and cause hemolysis.
- Disseminated intravascular coagulation (DIC): DIC is a condition characterized by widespread activation of the blood clotting process, which can lead to the formation of blood clots in small blood vessels. These clots can damage red blood cells and cause hemolysis.
- Malignant hypertension: Malignant hypertension is a severe form of high blood pressure that can damage small blood vessels throughout the body, leading to hemolysis.
- HELLP syndrome: HELLP syndrome is a complication of pregnancy characterized by hemolysis, elevated liver enzymes, and low platelet count. The exact cause of HELLP syndrome is not fully understood, but it is believed to be related to abnormalities in the placenta.
- Autoimmune disorders: Some autoimmune disorders, such as systemic lupus erythematosus (SLE) and antiphospholipid syndrome, can cause the formation of antibodies that attack red blood cells, leading to hemolysis.
- Cancer: Certain cancers, such as leukemia or lymphoma, can lead to the formation of blood clots in small blood vessels, which can damage red blood cells and cause hemolysis.
- Infections: Infections, particularly those caused by bacteria such as Escherichia coli (E. coli) or Shigella, can trigger a response in the immune system that leads to the formation of blood clots and hemolysis.
- Certain medications: Some medications, such as chemotherapeutic agents or certain antibiotics, can cause hemolysis as a side effect.
- Severe burns: Severe burns can damage blood vessels and lead to the formation of blood clots, which can cause hemolysis.
Treatment of MAHA focuses on addressing the underlying cause and managing symptoms. Prompt diagnosis and treatment are essential to prevent further complications and improve outcomes.
What is the treatment for microangiopathic hemolytic anemia?
The treatment for microangiopathic hemolytic anemia (MAHA) depends on the underlying cause of the condition. Treatment aims to address the cause of the hemolysis, manage symptoms, and prevent complications. Some general treatment approaches for MAHA may include:
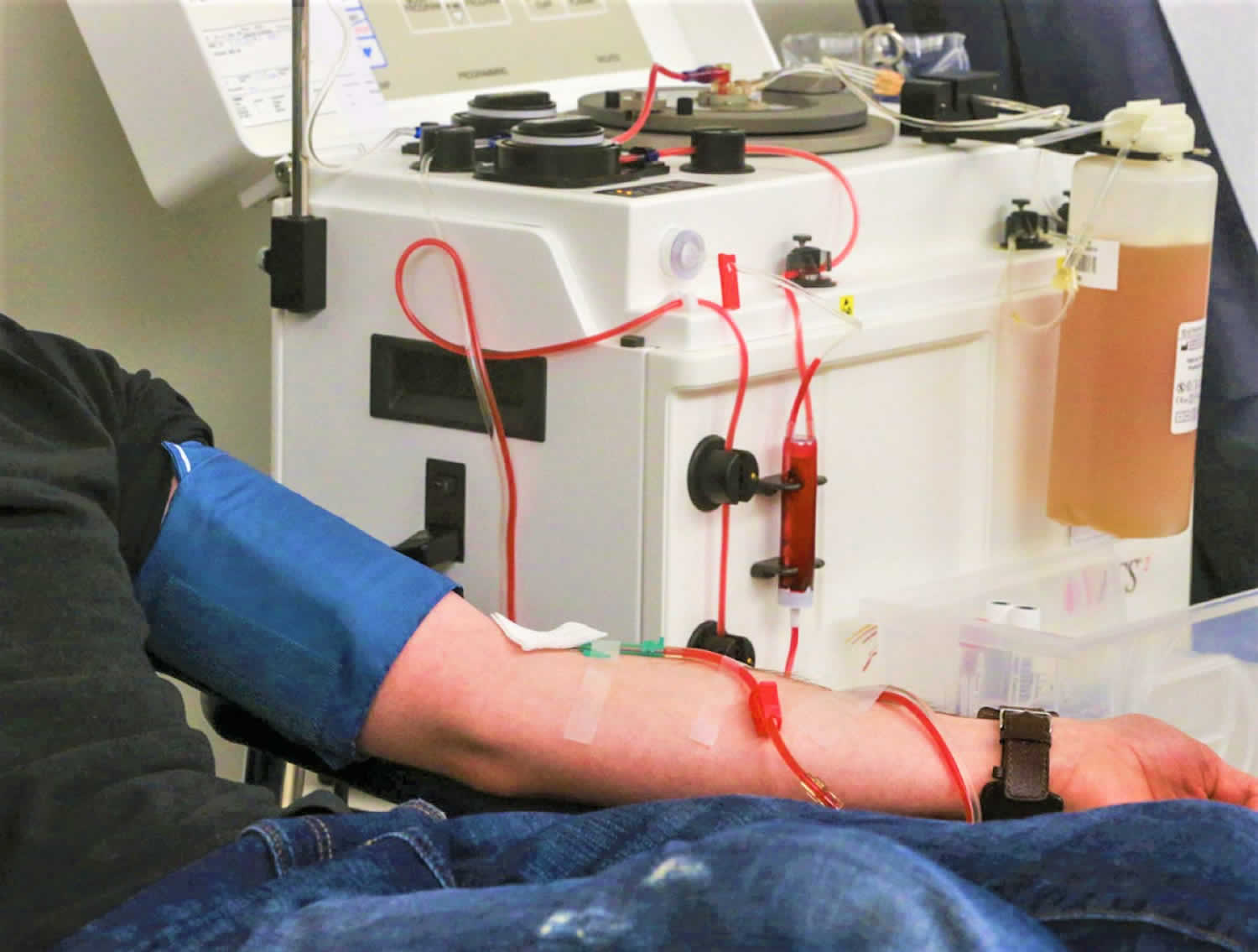
- Plasma exchange (plasmapheresis): Plasma exchange is a procedure in which the liquid portion of the blood (plasma) is removed and replaced with a replacement solution. This can help remove circulating antibodies or other factors that are causing the hemolysis.
- Corticosteroids: Corticosteroids, such as prednisone, may be used to suppress the immune system and reduce the production of antibodies that are attacking red blood cells.
- Immunosuppressive therapy: In cases where the underlying cause of MAHA is an autoimmune disorder, immunosuppressive medications may be used to suppress the immune response and reduce hemolysis.
- Blood transfusions: In severe cases of MAHA, blood transfusions may be necessary to replace the red blood cells that have been destroyed.
- Treatment of underlying conditions: If MAHA is caused by an underlying condition, such as thrombotic thrombocytopenic purpura (TTP) or hemolytic uremic syndrome (HUS), treatment will focus on managing that condition. This may include medications to prevent blood clot formation or treatment for infections.
- Splenectomy: In some cases, surgical removal of the spleen (splenectomy) may be necessary to reduce the destruction of red blood cells. This is more commonly done in cases of hereditary MAHA, such as hereditary spherocytosis.
- Anticoagulant therapy: In cases where blood clot formation is contributing to hemolysis, anticoagulant medications may be used to prevent further clot formation.
- Supportive care: Supportive care may include measures to manage symptoms such as pain, fatigue, and shortness of breath. This may involve medications, physical therapy, or other interventions.
It is important for individuals with MAHA to receive prompt and appropriate treatment to prevent complications and improve outcomes. Treatment should be tailored to the specific needs of each individual based on the underlying cause of MAHA and other factors. Close monitoring by a healthcare provider is essential to ensure that treatment is effective and to address any complications that may arise.