Pulmonary Arterial Hypertension: Symptoms, Causes, Treatment
What are the symptoms of pulmonary arterial hypertension?
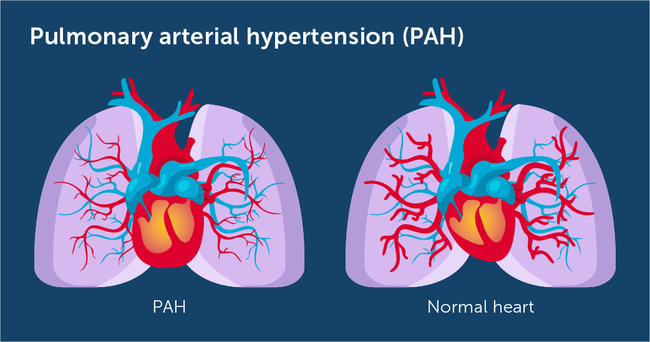
Pulmonary arterial hypertension (PAH) is a rare, progressive disorder characterized by high blood pressure in the arteries of the lungs. Symptoms of PAH can vary depending on the stage of the disease and may include:
- Shortness of breath: Initially with exertion, but eventually at rest as the disease progresses.
- Fatigue: Feeling tired or weak, often due to decreased oxygen levels in the blood.
- Chest pain: A dull, aching pain in the chest, especially during physical activity.
- Dizziness or fainting: Especially with exertion, due to decreased oxygen levels in the blood.
- Swelling (edema): Particularly in the ankles, legs, or abdomen, due to fluid retention.
- Palpitations: Sensations of rapid, fluttering, or pounding heartbeats.
- Bluish lips or skin (cyanosis): Due to low oxygen levels in the blood.
- Dry cough: Which may worsen over time.
- Decreased appetite: And unintentional weight loss.
It’s important to note that the symptoms of PAH can be nonspecific and may overlap with other conditions. PAH is a serious condition that requires prompt diagnosis and treatment by a healthcare professional experienced in managing the disease. If you or a loved one are experiencing symptoms suggestive of PAH, it’s important to seek medical evaluation from a healthcare provider for an accurate diagnosis and appropriate management.
What are the causes of pulmonary arterial hypertension?
Pulmonary arterial hypertension (PAH) can be idiopathic (of unknown cause), heritable, or associated with other conditions. The exact cause of idiopathic PAH is not fully understood, but it is believed to involve a combination of genetic, environmental, and other factors. Heritable PAH is caused by genetic mutations that affect the function of the pulmonary arteries. Associated PAH can be caused by a variety of underlying conditions and risk factors, including:
- Connective tissue diseases: Conditions such as scleroderma, lupus, and rheumatoid arthritis can be associated with PAH.
- Congenital heart disease: Some congenital heart defects can lead to PAH, especially if they involve abnormalities of the pulmonary arteries or veins.
- Liver disease: Certain liver diseases, such as cirrhosis, can lead to PAH.
- HIV infection: HIV can be associated with PAH, although the exact mechanism is not fully understood.
- Drugs and toxins: Certain medications and toxins, such as appetite suppressants and illicit drugs, can increase the risk of developing PAH.
- Schistosomiasis: Infection with the parasite Schistosoma can lead to PAH, especially in endemic regions.
- Genetic predisposition: While most cases of PAH are not inherited, there may be a genetic predisposition to the condition in some individuals.
- Other conditions: PAH can also be associated with conditions such as chronic obstructive pulmonary disease (COPD), sleep apnea, and high altitudes.
It’s important to note that while these factors can increase the risk of developing PAH, not everyone with these risk factors will develop the condition. PAH is a complex disorder with multiple contributing factors, and more research is needed to fully understand its causes and risk factors.
What is the treatment for pulmonary arterial hypertension?
The treatment for pulmonary arterial hypertension (PAH) aims to improve symptoms, slow disease progression, and improve quality of life. Treatment options may include:
- Medications: Several classes of medications are used to treat PAH, including:
- Vasodilators: Drugs that relax and widen the blood vessels in the lungs, such as calcium channel blockers, prostacyclin analogs (e.g., epoprostenol, treprostinil), and endothelin receptor antagonists (e.g., bosentan, ambrisentan).
- Phosphodiesterase-5 (PDE-5) inhibitors: Drugs that help relax blood vessels, such as sildenafil and tadalafil.
- Guanylate cyclase stimulators: Drugs that help relax blood vessels, such as riociguat.
- Oxygen therapy: Supplemental oxygen may be prescribed to improve oxygen levels in the blood and reduce the workload on the heart.
- Diuretics: Medications to reduce fluid retention and swelling (edema) in the body.
- Anticoagulants: Medications to prevent blood clots, which can be a complication of PAH.
- Exercise training: Supervised exercise programs may be recommended to improve exercise capacity and quality of life.
- Lung transplant: In severe cases of PAH that do not respond to other treatments, lung transplantation may be considered.
- Supportive therapies: Additional therapies such as nutritional support, counseling, and psychological support may be beneficial in managing PAH.
It’s important for individuals with PAH to work closely with a healthcare team experienced in managing the condition to develop a personalized treatment plan. Treatment may need to be adjusted over time based on the individual’s response to therapy and the progression of the disease. Regular monitoring and follow-up care are essential for managing PAH effectively.