Respiratory Problems
What are some common lung problems?
There are several common respiratory problems that can affect the lungs and respiratory system. Some of the most common respiratory problems include:
What is asthma and what is its treatment?
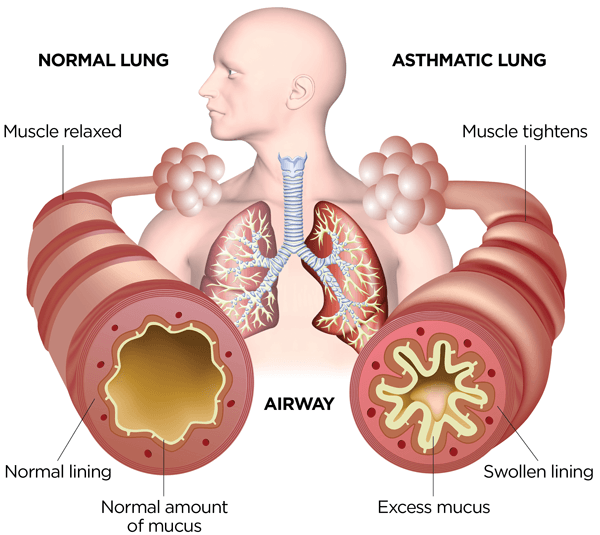
Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, leading to symptoms such as wheezing, coughing, shortness of breath, and chest tightness. These symptoms can range from mild to severe and can be triggered by various factors, including allergens, respiratory infections, exercise, and irritants such as smoke or strong odors.
The treatment of asthma aims to control symptoms, prevent exacerbations, and improve quality of life. Treatment typically involves a combination of medications and lifestyle modifications. Here are some common components of asthma treatment:
- Bronchodilators: These medications help to relax the muscles around the airways, making it easier to breathe. Short-acting bronchodilators, such as albuterol, are used to relieve acute symptoms, while long-acting bronchodilators are used to provide ongoing control.
- Inhaled corticosteroids: These medications reduce inflammation in the airways, helping to prevent asthma symptoms. They are often used as a maintenance treatment in people with persistent asthma.
- Combination inhalers: Some medications combine a corticosteroid with a long-acting bronchodilator in a single inhaler. These medications can help improve asthma control by addressing both inflammation and bronchoconstriction.
- Leukotriene modifiers: These medications block the action of leukotrienes, substances in the body that can cause inflammation and constriction of the airways. They are used as a maintenance treatment in some people with asthma.
- Immunomodulators: These medications, such as omalizumab, are used in people with severe asthma that is not well controlled with other medications. They work by targeting specific immune system proteins involved in asthma inflammation.
- Lifestyle modifications: Avoiding triggers, such as allergens or irritants, can help reduce the frequency and severity of asthma symptoms. Additionally, regular physical activity and maintaining a healthy weight can help improve overall lung function and asthma control.
It’s important for people with asthma to work closely with their healthcare provider to develop a personalized asthma action plan. This plan should include information on how to recognize worsening symptoms, when to seek medical help, and how to adjust medication dosages based on symptoms and peak flow measurements. Regular follow-up appointments are also important to monitor asthma control and adjust treatment as needed.
What is chronic obstructive pulmonary disease, and what is its treatment?
Chronic obstructive pulmonary disease (COPD) is a chronic inflammatory lung disease that causes obstructed airflow from the lungs. The main symptoms include shortness of breath, cough, and sputum production. COPD is most commonly caused by smoking, but other factors such as air pollution, genetic factors, and respiratory infections can also contribute to its development.
Treatment for COPD aims to relieve symptoms, improve quality of life, and slow the progression of the disease. The main components of COPD treatment include:
- Smoking cessation: Quitting smoking is the most important step in managing COPD and slowing its progression. Smoking cessation programs and medications can help people quit smoking.
- Bronchodilators: These medications help to relax the muscles around the airways, making it easier to breathe. They can be short-acting (used for symptom relief) or long-acting (used for maintenance treatment).
- Inhaled corticosteroids: These medications reduce inflammation in the airways and are used to reduce exacerbations in people with more severe COPD.
- Pulmonary rehabilitation: This program includes exercise training, education, and counseling to help improve lung function, exercise capacity, and quality of life in people with COPD.
- Oxygen therapy: Supplemental oxygen therapy may be prescribed for people with severe COPD who have low levels of oxygen in their blood.
- Surgery: In some cases, surgery such as lung volume reduction surgery or lung transplantation may be recommended for people with severe COPD.
- Vaccinations: Vaccinations against influenza and pneumonia can help prevent respiratory infections, which can exacerbate COPD symptoms.
It’s important for people with COPD to work closely with their healthcare provider to develop a personalized treatment plan. This plan should include regular monitoring of symptoms, lung function, and exacerbations, as well as adjustments to treatment as needed. By following their treatment plan and making lifestyle changes, people with COPD can effectively manage their symptoms and improve their quality of life.
What is pneumonia, and what is its treatment?
Pneumonia is an infection that inflames the air sacs in one or both lungs. The air sacs may fill with fluid or pus (purulent material), causing cough with phlegm or pus, fever, chills, and difficulty breathing. Pneumonia can range in severity from mild to life-threatening and is most serious for infants and young children, people older than age 65, and people with weakened immune systems.
The treatment for pneumonia depends on the underlying cause of the infection, the severity of symptoms, and the overall health of the individual. In most cases, pneumonia can be treated at home with the following measures:
- Antibiotics: If the pneumonia is caused by bacteria, antibiotics are used to treat the infection. It’s important to take the full course of antibiotics prescribed by your healthcare provider, even if you start to feel better.
- Antiviral medications: If the pneumonia is caused by a virus, such as influenza (flu), antiviral medications may be prescribed. These medications are most effective when started within 48 hours of the onset of symptoms.
- Fever reducers: Over-the-counter medications such as acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) can help reduce fever and relieve pain.
- Cough medicine: Cough medicine may be recommended to help alleviate coughing and make it easier to breathe.
- Fluids: It’s important to stay hydrated by drinking plenty of fluids, such as water, juice, or soup.
- Rest: Getting plenty of rest allows the body to focus on fighting the infection.
In more severe cases of pneumonia, especially in older adults or those with weakened immune systems, hospitalization may be required. In the hospital, treatment may include intravenous (IV) antibiotics, oxygen therapy, and respiratory therapy.
Prevention of pneumonia includes practicing good hygiene, getting vaccinated (especially for influenza and pneumococcal pneumonia), and avoiding smoking and exposure to secondhand smoke. If you suspect you have pneumonia, it’s important to see a healthcare provider for proper diagnosis and treatment.
What is bronchitis, and what is its treatment?
Bronchitis is an inflammation of the lining of the bronchial tubes, which carry air to and from the lungs. Acute bronchitis is usually caused by viruses, most commonly the same viruses that cause colds and flu (influenza). Chronic bronchitis is a type of chronic obstructive pulmonary disease (COPD) characterized by a persistent cough that produces sputum (phlegm) and lasts for at least three months, with recurring bouts occurring for at least two consecutive years.
Treatment for bronchitis depends on whether it is acute or chronic:
- Acute bronchitis: Most cases of acute bronchitis are caused by viral infections and do not require antibiotics. Treatment focuses on relieving symptoms and may include rest, plenty of fluids, and over-the-counter medications to relieve cough and fever. In some cases, a healthcare provider may prescribe an inhaler to help open the airways and reduce wheezing.
- Chronic bronchitis: Treatment for chronic bronchitis aims to relieve symptoms, prevent complications, and slow the progression of the disease. This may include medications such as bronchodilators to help open the airways, inhaled steroids to reduce inflammation, and antibiotics if there is a bacterial infection. Pulmonary rehabilitation, which includes exercise training, education, and counseling, can also be beneficial for people with chronic bronchitis.
In addition to medical treatment, lifestyle changes can help manage bronchitis:
- Quit smoking: Smoking is the leading cause of chronic bronchitis and quitting smoking can help slow the progression of the disease.
- Avoid irritants: Avoid exposure to lung irritants, such as smoke, dust, and fumes, which can worsen bronchitis symptoms.
- Stay hydrated: Drink plenty of fluids to help loosen mucus and make it easier to cough up.
- Use a humidifier: Using a humidifier can help moisten the air, making it easier to breathe.
It’s important to see a healthcare provider if you have symptoms of bronchitis, especially if you have a persistent cough, fever, or difficulty breathing. A healthcare provider can determine the cause of your symptoms and recommend appropriate treatment.
What is the flu, and what is its treatment?
The flu, or influenza, is a contagious respiratory illness caused by influenza viruses. It can cause mild to severe illness and can lead to serious complications, especially in young children, older adults, and people with certain underlying health conditions.
Symptoms of the flu can include fever, cough, sore throat, runny or stuffy nose, body aches, headache, chills, and fatigue. Treatment for the flu typically focuses on relieving symptoms and preventing complications. Here are some common treatments for the flu:
- Antiviral medications: Prescription antiviral drugs, such as oseltamivir (Tamiflu), zanamivir (Relenza), and peramivir (Rapivab), can help reduce the severity and duration of flu symptoms if taken within the first 48 hours of illness. These medications work by preventing the virus from reproducing in the body.
- Over-the-counter medications: Over-the-counter medications, such as acetaminophen (Tylenol) or ibuprofen (Advil, Motrin), can help reduce fever and relieve body aches and headache. It’s important to follow the dosing instructions on the label and consult a healthcare provider before giving these medications to children.
- Fluids: Drinking plenty of fluids, such as water, juice, or broth, can help prevent dehydration and loosen mucus.
- Rest: Getting plenty of rest allows the body to focus on fighting the infection and can help speed up recovery.
- Symptom relief: Using a humidifier, gargling with salt water, and using throat lozenges or cough drops can help relieve sore throat and cough.
- Prevention: The best way to prevent the flu is by getting an annual flu vaccine. Other preventive measures include washing hands frequently, avoiding close contact with sick individuals, and staying home when sick to prevent spreading the virus to others.
In some cases, the flu can lead to complications such as pneumonia, so it’s important to seek medical attention if you have severe symptoms, difficulty breathing, persistent chest pain, or sudden dizziness. Your healthcare provider can determine the best course of treatment based on your symptoms and medical history.
What is a pulmonary embolism, and what is its treatment?
A pulmonary embolism (PE) is a serious condition that occurs when a blood clot (usually from the leg) travels to the lungs and blocks a pulmonary artery or one of its branches. This blockage can prevent blood from reaching parts of the lung, leading to damage to lung tissue and potentially life-threatening complications.
Symptoms of a pulmonary embolism can vary but may include sudden shortness of breath, chest pain (which may worsen with deep breaths), rapid heart rate, cough (sometimes with bloody sputum), and lightheadedness or fainting.
Treatment for a pulmonary embolism typically involves:
- Anticoagulant medications: These medications, also known as blood thinners, are used to prevent new blood clots from forming and to prevent existing blood clots from getting bigger. Commonly used anticoagulants include heparin and warfarin (Coumadin), as well as newer oral anticoagulants such as rivaroxaban (Xarelto) and apixaban (Eliquis).
- Thrombolytic therapy: In some cases, especially if the pulmonary embolism is large or causing severe symptoms, thrombolytic medications (such as alteplase or tenecteplase) may be used to dissolve the blood clot quickly. This treatment carries a risk of bleeding and is typically reserved for severe cases.
- Surgery: In rare cases, surgery may be necessary to remove a large blood clot from the pulmonary artery. This procedure, known as pulmonary embolectomy, is considered when other treatments are not effective or are not possible.
- Inferior vena cava (IVC) filter: For people who are unable to take anticoagulant medications or who continue to have blood clots despite treatment, an IVC filter may be placed in the inferior vena cava (the large vein that carries blood from the lower body to the heart) to catch blood clots before they reach the lungs.
- Supportive care: Supportive measures, such as oxygen therapy and pain management, may be used to relieve symptoms and help the person breathe more easily.
It’s important to seek immediate medical attention if you experience symptoms of a pulmonary embolism, as prompt treatment can help prevent serious complications and improve outcomes. Treatment for a pulmonary embolism is tailored to the individual and depends on the size and location of the blood clot, the person’s overall health, and other factors.
What is lung cancer, and what is its treatment?
Lung cancer is a type of cancer that starts in the lungs. It is the leading cause of cancer-related deaths worldwide. There are two main types of lung cancer: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). NSCLC is the most common type, accounting for about 85% of all lung cancers, while SCLC accounts for about 15%.
Treatment for lung cancer depends on several factors, including the type and stage of the cancer, the person’s overall health, and their preferences. Treatment options may include:
- Surgery: Surgery may be used to remove the tumor and a portion of surrounding healthy tissue. It is most effective when the cancer is diagnosed at an early stage and has not spread beyond the lungs.
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells or stop them from growing. It is often used in combination with surgery or radiation therapy for NSCLC and is the primary treatment for SCLC.
- Radiation therapy: Radiation therapy uses high-energy rays to kill cancer cells. It may be used alone or in combination with surgery or chemotherapy.
- Targeted therapy: Targeted therapy drugs target specific abnormalities present in cancer cells. They are used to treat NSCLC that has certain genetic mutations.
- Immunotherapy: Immunotherapy drugs help the immune system recognize and attack cancer cells. They are used to treat NSCLC and SCLC that has spread to other parts of the body.
- Palliative care: Palliative care focuses on providing relief from symptoms and improving quality of life for people with advanced lung cancer. It can be used alongside other treatments or as the main approach to care.
The choice of treatment depends on the stage of the cancer, the person’s overall health, and their preferences. A multidisciplinary team of healthcare providers, including oncologists, surgeons, radiation oncologists, and other specialists, work together to develop a treatment plan that is tailored to each individual. Early detection and treatment can improve outcomes for people with lung cancer, so it’s important to see a healthcare provider if you have symptoms such as persistent cough, chest pain, or unexplained weight loss.
What is pulmonary hypertension, and what is its treatment?
Pulmonary hypertension (PH) is a type of high blood pressure that affects the arteries in the lungs and the right side of the heart. It occurs when the walls of the pulmonary arteries become thickened or narrowed, making it harder for blood to flow through the lungs and causing increased pressure in the pulmonary arteries.
There are several types of pulmonary hypertension, which are classified based on the underlying cause. Treatment for pulmonary hypertension depends on the type and severity of the condition, as well as the underlying cause.
- Medications: Several classes of medications are used to treat pulmonary hypertension, including:
- Vasodilators: These medications relax and widen the blood vessels, reducing pressure in the pulmonary arteries. Examples include calcium channel blockers, prostacyclin analogs (such as epoprostenol, treprostinil, and iloprost), and phosphodiesterase-5 inhibitors (such as sildenafil and tadalafil).
- Endothelin receptor antagonists: These medications block the action of endothelin, a substance that can narrow blood vessels. Examples include bosentan, ambrisentan, and macitentan.
- Diuretics: Diuretics may be used to reduce fluid buildup in the body, which can be helpful in some cases of pulmonary hypertension.
- Oxygen therapy: Supplemental oxygen therapy may be recommended for people with pulmonary hypertension who have low oxygen levels in their blood.
- Surgery: In some cases, surgery may be necessary to treat underlying causes of pulmonary hypertension or to improve blood flow in the lungs. This may include procedures such as atrial septostomy (creating a hole in the wall between the heart’s upper chambers) or lung transplantation.
- Lifestyle changes: Lifestyle changes, such as quitting smoking, maintaining a healthy weight, and staying active, can help improve symptoms and overall health in people with pulmonary hypertension.
- Regular monitoring: People with pulmonary hypertension require regular monitoring by a healthcare provider to assess the effectiveness of treatment and make any necessary adjustments.
The goal of treatment for pulmonary hypertension is to reduce symptoms, improve quality of life, and slow the progression of the disease. Treatment is typically lifelong and requires close collaboration between the person with pulmonary hypertension and their healthcare team. Early diagnosis and treatment can help improve outcomes for people with pulmonary hypertension.
What is cystic fibrosis, and what is its treatment?
Cystic fibrosis (CF) is a genetic disorder that affects the lungs, digestive system, and other organs. It causes the production of thick, sticky mucus that can clog the airways and lead to life-threatening lung infections. CF also affects the pancreas, causing difficulty digesting food and absorbing nutrients.
Treatment for cystic fibrosis focuses on managing symptoms, preventing complications, and improving quality of life. Treatment options may include:
- Airway clearance techniques: These techniques help to loosen and clear mucus from the lungs, making it easier to breathe. They may include chest physiotherapy, using a vibrating vest, or using a handheld device to help clear mucus.
- Medications: Medications may be used to thin mucus, reduce inflammation in the airways, and prevent or treat lung infections. Common medications include:
- Bronchodilators: These medications help to open the airways, making it easier to breathe.
- Mucolytics: These medications help to thin mucus, making it easier to clear from the lungs.
- Antibiotics: Antibiotics may be used to treat lung infections, which are common in people with CF.
- Pancreatic enzyme replacement therapy (PERT): PERT is used to help people with CF digest food and absorb nutrients. It involves taking pancreatic enzyme capsules with meals and snacks to replace the enzymes that the pancreas is unable to produce.
- Nutritional therapy: A high-calorie, high-protein diet is often recommended for people with CF to help maintain a healthy weight and support growth and development.
- Lung transplant: In some cases, a lung transplant may be recommended for people with severe lung disease that does not respond to other treatments.
- Gene therapy: Gene therapy is a promising area of research for CF, aimed at correcting the underlying genetic defect that causes the disease. Clinical trials are ongoing to evaluate the safety and effectiveness of gene therapy for CF.
It’s important for people with CF to work closely with a multidisciplinary healthcare team, including pulmonologists, dietitians, respiratory therapists, and social workers, to develop a comprehensive treatment plan. With proper management, people with CF can lead relatively normal lives and maintain good overall health.
What is sleep apnea, and what is its treatment?
Sleep apnea is a sleep disorder characterized by pauses in breathing or shallow breaths during sleep. These pauses can last from a few seconds to minutes and can occur multiple times per hour. There are two main types of sleep apnea: obstructive sleep apnea, which occurs when the throat muscles relax and block the airway, and central sleep apnea, which occurs when the brain fails to send signals to the muscles that control breathing.
Treatment for sleep apnea depends on the type and severity of the condition. Common treatments include:
- Continuous positive airway pressure (CPAP) therapy: CPAP is the most common and effective treatment for obstructive sleep apnea. It involves wearing a mask over the nose or nose and mouth during sleep, which delivers a continuous flow of air to keep the airway open.
- Oral appliances: Oral appliances are devices that are worn in the mouth during sleep to help keep the airway open. They are typically used for mild to moderate obstructive sleep apnea or for people who cannot tolerate CPAP therapy.
- Lifestyle changes: Making lifestyle changes, such as losing weight, avoiding alcohol and sedatives before bedtime, and sleeping on your side instead of your back, can help reduce symptoms of sleep apnea.
- Surgery: In some cases, surgery may be recommended to treat sleep apnea. Surgical options may include removing excess tissue from the throat, repositioning the jaw, or implanting a device to stimulate the muscles that control breathing.
- Treatment for underlying conditions: If sleep apnea is caused by underlying conditions, such as nasal congestion or hypothyroidism, treating these conditions may help improve symptoms of sleep apnea.
It’s important to seek treatment for sleep apnea, as untreated sleep apnea can lead to serious complications, including high blood pressure, heart disease, stroke, and daytime fatigue. If you suspect you have sleep apnea, talk to your healthcare provider about undergoing a sleep study to diagnose the condition and determine the best course of treatment.
These are just a few examples of common respiratory problems. It’s important to seek medical attention if you experience any symptoms of respiratory problems, as early diagnosis and treatment can help prevent complications and improve outcomes.